United Kingdom
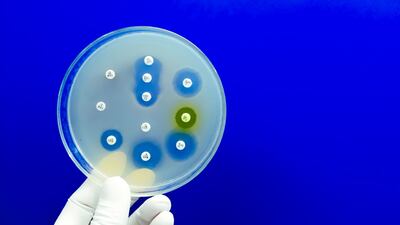
The UK will require all antibiotic manufacturers looking to apply for funding under its subscription payment model to demonstrate they are meeting waste discharge standards in a bid to reduce antimicrobial resistance.
Pharmaceutical companies should only use AI in evidence generation and reporting where there is “demonstrable value from doing so,” according to England’s health technology assessment body, NICE.
While the drug regulator has approved Eisai/Biogen’s early Alzheimer’s disease treatment, the health technology assessment institute is worried that its benefits are too small to justify its costs – a concern that Eisai has pledged to address.
It is “absolutely fundamental” that manufacturers of cell and gene therapies interact with inspectors from regulatory agencies to understand their expectations around good manufacturing practice, a compliance consultant at CDMO eXmoor pharma says.
The MHRA says that having a complete picture of all upcoming filings will allow it to ensure “consistent and predictable” timelines for assessments and identify “potentially transformative technologies” at an early stage.
Brexit has been cited as a cause of the UK’s 2020 decline in clinical trials, but research suggests that other global trends including the pandemic also had a large impact. Meanwhile, the MHRA’s efforts to incentivize sponsors could boost trial figures “substantially,” an expert says.
In this third article of a series on new drug reimbursement recommendations by the HTA body NICE, the Pink Sheet finds that fewer innovative medicines are reimbursed in England than in eight other European nations.
It appears that the complexity of dealing with older products under the VPAG is the main cause of delays at the health department in sharing reference prices with pharma companies.
Casgevy, the world’s first CRISPR gene editing therapy, is the second drug to be accepted onto a managed access scheme via England’s Innovative Medicines Fund, offering a new treatment for patients with transfusion-dependent beta thalassemia.
Sanofi, Alexion and Eli Lilly argue for changes in England’s health technology assessment and medicine pricing processes that could help patients to access more medicines.
The UK and EU pharma industry associations have defended their respective codes of practice despite alarming study results. Meanwhile, a consultation on proposals to revise the UK code received over 3,500 comments.
Since 2019, 91 health technology assessments have been terminated by England’s NICE because companies withdrew their applications or did not submit evidence. In the first of this three-part article series, pharma firms share their reasons for opting out of the process.
England’s NICE has “misclassified” HER2-low metastatic breast cancer as a medium severity disease, say AstraZeneca and Daiichi Sankyo, the co-developers of Enhertu. NICE said it would consider a rapid re-appraisal if the companies offered a “fair price” for the drug.
A new UK network, led by an expert who has also worked on high-level EU data projects, has been established to test whether a common data model could help to facilitate real-world evidence studies by increasing the “usability” of data.
The UK’s drug regulator said that a trial run by cell therapy firm Celixir “risked seriously jeopardizing the rights, safety and wellbeing of trial participants” after an inspection discovered expired product batches, unauthorized dosing and other serious breaches.
Establishing multi-site network centers for rare diseases can help advance clinical research, but “onerous” regulatory compliance issues are a barrier that must be overcome, a clinical academic says.
A UK-based CRO specializing in human challenge trials says there is a big shift in industry sentiment towards such studies. Companies targeting infectious diseases are now actively accommodating challenge trials in their development plans instead of needing persuasion.
A prominent rare disease researcher has praised the UK’s Department for Health and Social Care for its transparency and willingness to work with experts, but said that regulatory systems needed to speed up to facilitate patient access to innovative treatments.
Market exclusivity is the key incentive offered under the EU orphan drug framework, but pricing and regulatory problems are the main challenges for rare disease drugmakers, not the pressure from competitors, a life sciences lawyer says.
The latest report on the competitiveness of the UK’s life sciences sector shows that the nation “continues to underperform” on its potential in terms of the adoption of new treatments and innovation, according to industry body the ABPI.