Reimbursement
Industry says it is ready to work with the government on the recommendations from a major review of Australia’s health technology assessment system that covers areas such as discount rate reductions and setting up a separate budgetary allocation to temporarily subsidize access to certain drugs.
Multi-cancer diagnostics can help get oncology patients the treatment they need more quickly, but lack of reimbursement has kept such tests out of reach for many patients. Bills providing coverage have passed or are under consideration in more than half of the states and have been introduced in both houses of US Congress.
Medicare coverage with evidence development final guidance includes few substantive changes from the proposed version despite biopharma stakeholder concerns.
Pharmaceutical companies should only use AI in evidence generation and reporting where there is “demonstrable value from doing so,” according to England’s health technology assessment body, NICE.
While the drug regulator has approved Eisai/Biogen’s early Alzheimer’s disease treatment, the health technology assessment institute is worried that its benefits are too small to justify its costs – a concern that Eisai has pledged to address.
Congressional Budget Office responses to questions from US lawmakers on pharmacy benefit managers could add to the momentum for PBM reforms to go further than the current leading proposals.
William Audeh, chief medical officer at Agendia, is optimistic about study results suggesting the company’s genomic test MammaPrint, designed to predict which women with early-stage HR+ breast cancer are at risk of recurrence, also can be used to determine those that would benefit from extended endocrine therapy.
But the amount of savings realized when the Medicare negotiated prices go into effect in 2026 remains the subject of debate.
CBO estimated Medicare would get 50% net price reductions under the IRA, but CMS actually garnered 22%. The CBO analysis could not account for some of the particulars of the negotiations, but some health policy experts stressed any net gain over private Part D plan negotiation is a win.
Some manufacturers may have the dubious distinction of being targeted in the first and second rounds of the negotiation program, but at least will be familiar with the process the next time.
The first round of US government drug price negotiations resulted in prices for 10 drugs that will lower aggregate net spending by 22%
Net per drug savings achieved by the negotiation process is unclear because many of the products already have significant rebates. The announcement also leaves much of the agency’s negotiation process in the dark.
The CMS supplemental reimbursement for the gene therapies is higher than usual for new technologies, but is similar to the formula used for antibiotics.
A Japanese approval for Lilly's Alzheimer's drug donanemab is expected soon following a positive recommendation from the MHLW. The ministry has also announced reimbursement prices for 12 new products including Fabhalta, along with price cuts for Tezspire, Dupixent and competitors following a review.
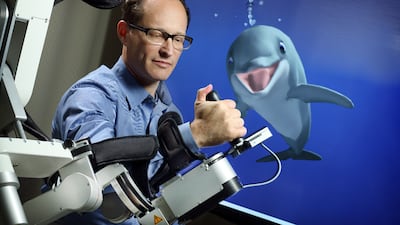
MindMaze seeks to create a beautiful immersive experience for patients recovering from brain injuries. Chief medical director John Krakauer, clearly a “Star Wars” fan, discusses the significant need for digital therapeutics at a time when therapists are in short supply, as well as the challenges facing the DTx space as a whole.
The analysis was released days before the Biden Administration is expected to announce a reduced Medicare Part D price for Johnson & Johnson’s immunosuppressant resulting from the government negotiation program established by the Inflation Reduction Act.
Avenda’s chief operating officer Brit Berry-Pusey spoke to Medtech Insight about the company’s CPT III code for its prostate cancer mapping AI and how regulatory bodies can align to support innovators.
Big Health announced it received FDA clearance for its digital therapeutics for insomnia and hopes a new CMS fee schedule will pave the way to reimbursement.
In this third article of a series on new drug reimbursement recommendations by the HTA body NICE, the Pink Sheet finds that fewer innovative medicines are reimbursed in England than in eight other European nations.
The long-awaited TCET final notice doesn’t address major concerns, medtech industry advocates say.
ADVERTISEMENT